Infectious diseases
Diseases where microbes are the immediate causes. This is because microbes can spread rapidly in the community.
Infectious agents:
Mostly microbes or micro-organisms such as bacteria, fungi, etc. have the ability to act as infectious agents.
Not all microbes are harmful to us. Pathogens are microbes harmful to humans, plants and animals.
- Virus: Common cold, influenza, dengue fever & AIDS.
- Bacteria: Typhoid fever, cholera, TB(tuberculosis), anthrax.
- Fungi: Many common skin infections.
- Protozoan: single-celled animals (Kingdom): Malaria & Kala Azar(a form of the disease leishmaniasis marked by emaciation, anaemia, fever, and enlargement of the liver and spleen)
Identification of the agent is very important in determining what kind of treatment to use. For example, Viruses live inside host cells, whereas bacteria rarely do; Viruses & bacterial multiply quickly, While worms multiply very slowly;
Means of Spread
The infections can spread through various modes of transmission:
- Air: sneeze: Tiny droplet nuclei carried in air currents for minutes to hours. For example, Common cold, pneumonia & TB. [Crowded living conditions are a problem]
- Water: If excreted from infectious gut disease suffering person, mixes with drinking water. For example, Cholera; [Likely to spread in the absence of safe supplies of drinking water]
- Sexual transmission: They are not spread by casual physical contact(handshake, hugs etc.), but can be spread through blood-to-blood contact(infected mother to baby through pregnancy or breastfeeding), by any action where any human cell can be physically transmitted. For example, Syphilis or AIDS.
- Animals/insects: carry infectious agents to potential hosts. These animals are intermediaries called vectors. For example, in mosquitoes, females need highly nutritious food in the form of blood to be able to lay mature eggs. They feed on warm-blooded animals, including humans; Rabies: Dog bite/ other animals.
Tissue-specific manifestations:
Different species of microbes seem to have evolved to home in on different parts of the body.
Entry points
This selection of a tissue is connected to its point of entry.
- Lungs: If they enter through the nose: Bacteria cause TB.
- Mouth: They can stay in the gut lining: For example, Typhoid-causing bacteria.
- Liver: Virus that causes Jaundice.
Infection with specific entry points can spread throughout the body. For example:
- HIV infection spreads to lymph nodes all over the body.
- Malaria-causing mosquito bites will go to the liver & then to RBC.
- Virus causing Japanese encephalitis, or brain fever: entry: mosquito bite, but infects the brain
Targetted tissue
Signs and symptoms depend on the targeted tissue or organ:
- Lungs: symptoms will be cough & breathlessness.
- Liver: There will be jaundice.
- Brain: Headache, vomiting, fits or unconsciousness.
Tissue-specific effects of infectious disease:
- The immune system is activated in response to infection: (active immune system) recruits many cells to the affected tissue to kill microbes. This recruitment process is called Inflammation.(causes local effects: swelling, pain; & general effects: fever)
- HIV: The virus goes to the immune system & damages its function. The body can’t fight off the many minor infections that we face every day. [Even a small cold can become pneumonia, minor gut infection can become diarrhoea with blood loss: Kills people]
Types of Infectious diseases
Communicable Disease:
Most diseases caused by microbes can be spread from organism to organism. These diseases are known as communicable diseases. They enter in body through air, water, food or sexual transmission and can be transmitted by direct contact or through vectors.
Vector-borne diseases
- Host: infected species.
- Reservoir: Where it can maintain itself until other susceptible hosts are infected/contacted.
- Infectious agent
- Carriers/Vectors: Vectors are animal intermediaries that carry infectious agents to potential hosts. For example, Flies, the Anopheles mosquito (carries parasite of malaria), and the Female Aedes mosquito(Dengue Virus). All mosquitoes breed in water.
Further, we will talk about zoonotic diseases which generally are carried by non-human hosts but sometimes jump into human pathology.
Disease in Animals:
- For example, Anthrax is dangerous for humans and cattle disease caused by a bacterium; [Robert Koch(1876) discovered Bacillus anthracis.
- Foot & mouth disease caused by a virus.
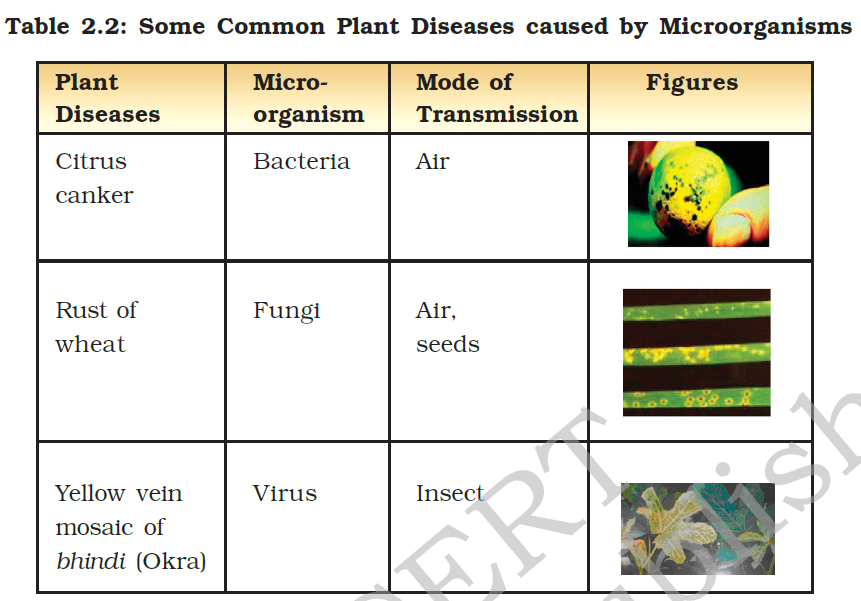
Disease in Plants:
- Certain chemicals can kill the microbes.
Diseases in Humans
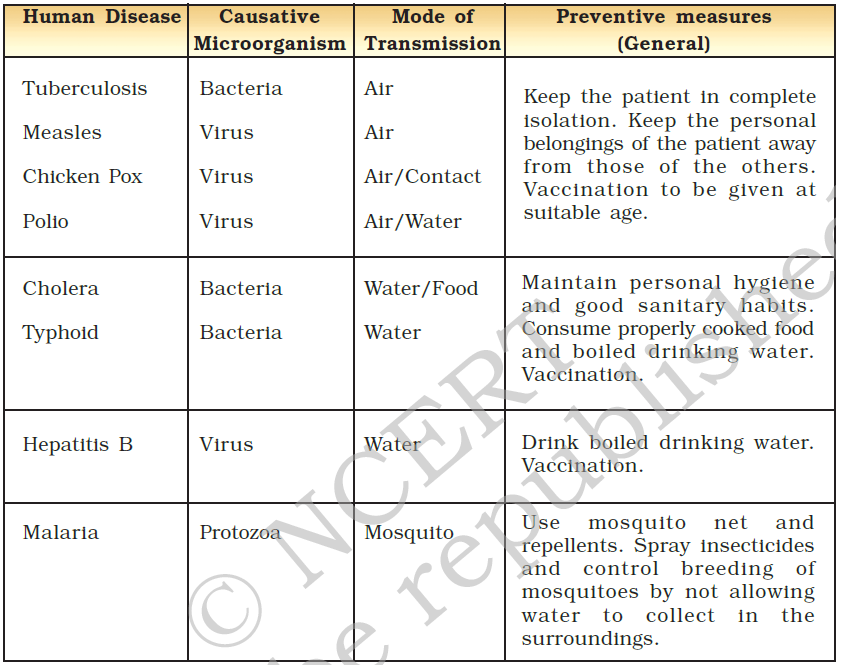
Here are a few common infectious illnesses that are caused by humans.
Food Poisoning: Caused by consumption of spoilt food (by microbes). Can cause illness/death.
Treatment of Infectious diseases
Antibiotics:
Anti-microbials are Drugs that block one of the life processes, that can be effective on one kind of microbe. Therefore, they kill or stop the growth of disease-causing microorganisms.
- Therefore, Antibiotics block biochemical pathways important for bacteria; For example, many bacteria make cell walls to protect themselves. Antibiotic penicillin blocks the bacterial processes that build cell walls. It doesn’t affect us much, we don’t have cell walls anyway.
- Similarly, we can block important chemical pathways of the fungi, and protozoa through anti-fungal etc.
- The number of them produced from bacteria & fungi. For example, Streptomycin, tetracycline & erythromycin;
These are consumed in various ways:
- Mixed with feed of livestock and poultry to check microbial infection in animals.
- Can be used to control many plant diseases.
However, viruses do not use these biochemical pathways at all; common cold, if it is along with bacterial infection, antibiotics can help. The viral part of the infection is unaffected by an antibiotic.
Principles of Treatment:
- Symptom-specific treatment: Reduce the symptoms(may not help in making microbe go away); They can help: reduce fever/pain/lose-motion: Take rest, and conserve energy so that it can be focused on healing.
- Microbe-specific treatment: Block essential biochemical pathways used by the microbes that are not essential for us.
- Viruses have very few biochemical pathways of their own, They enter our cells & use our machinery for their life processes. There are very few virus-specific targets to aim at. But there are significant advances: There is a drug that can keep HIV in control.
Limitation of Cure:
- After recovery, a few body functions might not be able to repair completely.
- Treatment may take time: the patient may be bedridden for some time.
- The person suffering from non-infectious disease can serve as a source from where infection may spread.
- The disease keeps spreading till even a few in a population are infected. The treatment of individuals does not stop this.
Antimicrobial resistance (AMR)
Antimicrobial resistance (AMR) is the ability of a microorganism (like bacteria, viruses, and some parasites) to stop an antimicrobial (such as antibiotics, antivirals and antimalarials) from working against it. Antibiotic Resistance is the most common form of AMR.
Problems caused by AMR:
- AMR can make even minor infections fatal.
- Complex surgeries such as organ transplantation and cardiac bypass might become more difficult to undertake because of untreatable infections and complications that may result post-surgery.
- No new class of antibiotics has been discovered in the past three decades.
- Social disparity: Antibiotics breed drug-resistant bacteria while poor and vulnerable have easy access to quality drugs; thus infections are not prevented from spreading in time.
A WHO report has predicted that anti-biotic resistance may cause a rise in the death of Indians to 20 lakhs/year by 2050.
Superbugs:
Often microbes become resistant to just a few anti-microbials. But in rare circumstances, they become resistant to almost all types ob bugs and become impossible to treat. Such a level of Anti-microbial resistance happens through two routes:
- Microbes inside the body develop a mutation in the genes spontaneously to fight a drug. These mutations take time to spread.
- Horizontal gene transfer: A microbe borrows resistance genes from its neighbours.
Reasons for AMR:
AMR is ultimately caused by negligence in industrial practice and at the policy level.
Human Negligence:
- Self–medication: People often rely on self-medication to basically avoid financial burdens.
- Easy Access to antibiotics without prescription through pharmacies and Informal healthcare providers as sources of healthcare further exacerbates the issue of self-medication.
- Prescription Risk: Anti-biotic prescription rate is high in the Private sector – a PHFI (Public Health Foundation of India) Report.
- Prevalent use of Spectrum of Antibiotics: due to Inadequate public sector diagnostic laboratories and affordability of private labs.
- Mass bathing is part of religious occasions.
Negligence by the Industry:
- Livestock: Antibiotics as growth promoters in food animals and poultry. Over 2/3rd of antibiotics manufactured by the pharmaceutical industry are used as growth promoters in the poultry and cattle industry.
- Environment Dumping: Effluents from the antibiotic manufacturing units are often dumped in sewage which pollutes rivers and lakes. When these drugs enter into soil and water, microbes grow resistant to them. However, the flow of genes from the environment to humans is a rare event. But once these genes jump into human pathology, they spread fast. Most transmission of genes happens from one human to another.
- Prevalence of various Hospital Associated Infections (also called nosocomial infections).
| Costilin Ban in 2019 |
Colistin: is now banned under the Drugs and Cosmetics Act, 1940, for manufacturing, sale and use in the Poultry industry. It is now mandatory for the manufacturers of antibiotic colistin to write clearly on the label that the drug is not to be used in food-producing animals, poultry, aqua farming and animal-feed supplements.
|
Policy initiative to counter Antimicrobial resistance
Several documents such as the Chennai Declaration of 2013 and the National Health Policy, 2017 have raised awareness of the superbug problem amongst the medical community and called for the holistic framework against AMR.
Regulations:
- National Policy for Containment of AMR 2011: Provided regulations for the use of antibiotics for humans.
- FSSAI guidelines.
- Health Ministry: amendments in Food Safety & Standards(Contaminants, Toxins & Residues) Regulations, 2011; To set permissible limits.
- The National Anti-Microbial Resistance Research and Surveillance Network (AMRRSN) was set up by ICMR to enable the compilation of National Data on AMR at different levels of Health Care.
Redline Campaign, 2016
The Redline Campaign was launched by the Ministry of Health and Family Welfare in 2016 to curb the irrational use of antibiotics and create awareness of the side effects of taking antibiotics without a prescription.
- All prescription-only antibiotics should be marked with a vertical red line on the packets: to curb over-the-counter sales. It means these should be consumed on the doctor’s advice and the patients need to complete the full course prescribed by the doctor.
- The sale of antibiotics and other antimicrobials over-the-counter is prevented by laws, but their weak enforcement in some countries and non-existent in many is a serious problem.
- Drugs and Cosmetic Rule, 1945 were amended in 2013 to incorporate a new Schedule H1 for this.
National Action Plan on Anti-Microbial Resistance (NAP-AMR)
In 2017, the government launched the NAP-AMR, with the following policy initiatives:
- One Health Approach: Assigned coordinated tasks to multiple government agencies involving health, education, environment, and livestock.
- To change prescription practices and consumer behaviour.
- Scale up infection control – Control.
- Antimicrobial Surveillance – Prevention.
- 2017 National action plan for AMR talks about limiting antibiotics in effluent being dumped by drug makers into the environment.
- It calls for states to develop state-level action plans to ensure on-the-ground implementation. States like Kerala, Madhya Pradesh and Delhi have formulated a State Action Plan for the Containment of AMR.
Global Initiatives against AMR
- WHO’s GAP-AMR 2015: Global Action Plan on AMR aims to optimize the use of antimicrobial medicines.
- Interagency Coordination Group on Antimicrobial Resistance (IACG) – initiated by the UN.
- It brings together partners across the UN, international organizations and individuals with expertise across human, animal and plant health, as well as the food, animal feed, trade, development and environment sectors, to formulate a blueprint for the fight against antimicrobial resistance.
- WHO provided the Secretariat for the IACG, with contributions from FAO and the World Organisation for Animal Health (OIE).
- IACG has recently released a report: “No Time to Wait: Securing The Future From Drug-Resistant Infections”, which highlights the financial fall-out of uncontrolled antimicrobial resistance.
- Global Antimicrobial Resistance Research and Development (AMRR&D) Hub: It was launched in 2018 in the 71st session of the World Health Assembly, following a call from G20 Leaders in 2017; India joined it in 2020.
- Aim: to address challenges and improve coordination and collaboration in global AMR R&D. It supports global priority setting and evidence-based decision-making on the allocation of resources for AMR R&D through the identification of gaps, overlaps and potential for cross-sectorial collaboration and leveraging in AMR R&D.
- Partners: the European Commission, two philanthropic foundations and four international organisations (as observers). The operation of the Global AMR R&D Hub is supported through a Secretariat, established in Berlin and is currently financed through grants from the German Federal Ministry of Education and Research (BMBF) and the Federal Ministry of Health (BMG).
- AWare Tool For Battling AMR: a new online tool developed by WHO which aims at guiding policymakers and health workers to use antibiotics safely and more effectively. It groups antibiotics into three main categories based on their strength and potential impact on Antimicrobial resistance (AMR).
- ‘Access’ antibiotics are first- or second-line treatments for common infections and should be widely accessible.
- ‘Watch’ category should be applied only to a limited group of well-defined syndromes.
- ‘Reserve’ category is the last resort to treat multi- or extensively-drug resistant bacteria.
- There is also a fourth category, ‘discouraged antibiotics’, which refers primarily to irrational antibiotic combinations that may negatively impact AMR and patient safety.
Prevention
Often Prevention is better than cure. We have to do this by two means:
- Public hygiene: Reduce exposure to means of spread such as through safe drinking water, clean environment and food. We can use food preservation techniques to slow or stop the growth of microbes altogether.
- Immunisation: Immune cells manage to kill off the infection long before it assumes major proportions.
- Small Pox: Famously, Edward Jenner(2 cent. Ago) realised that milkmaids who had cowpox didn’t catch smallpox even during epidemics. He tried deliberately giving cowpox to people, & found that they were now resistant to smallpox. Cow = Vacca (Latin); Vaccine derived from here. [Now smallpox is not common]
- Vaccine: We fool the immune system by giving a mimic of a microbe to develop immunity against a real one. For example, Tetanus, Diphtheria, whooping cough, measles, polio & others.
Food preservation:
Preventing food poisoning, by creating an adverse environment for microbes.
- Chemical method: Adding Preservatives; Salts & edible oils. For example, Pickle: Salt or acid preservatives., Sodium Benzoate & Sodium Meta bisulphite are common(also used in jams & squashes to check their spoilage.
- Common salt: used to preserve meat & fish for ages. Also to preserve amla, raw mangoes, tamarind (imli)
- Sugar: Jam, jellies squashes preserved by sugar. It reduces moisture content. Inhibits growth of Bacteria.
- Oil & Vinegar: Pickles: Bacteria can’t live in an acidic environment. Also Vegetable, fish, fruits & meat.
- Heat & Cold treatment: Kills many microbes; For example, Boiling milk, and keeping it in the fridge(inhibits growth). An even better method was developed by Louis Pasteur in the 19th century, known as Pasteurized milk. In this method, Milk is heated to 70oC for 15-30 seconds and then suddenly chilled and stored;
- Storage & Packing: Sealed air-tight packets to prevent the attack of microbes.
When disease-carrying microbe enters the body, the Body forms antibodies;
Immunisation
Immunisation refers to the process of creating antibodies that can fight the infectious disease.
Basics of Immunisation
- Antibodies:
- Specificity: The ability to distinguish different substances.
- Memory: the ability to respond more vigorously to repeated exposures to the same microbe.
- Lymphocytes: The cells that act as unique components of adaptive immunity. Antibodies secreted products of lymphocytes.
- Antigens: Foreign substances that induce specific immune responses or are recognized by lymphocytes or antibodies. Like Pathogen.
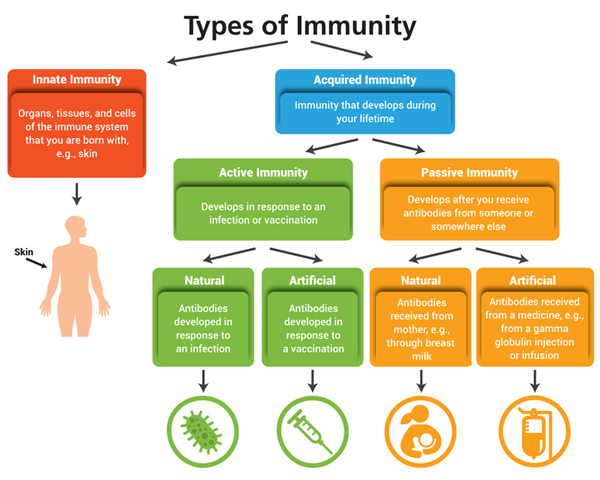
Two types of Immunities:
- Innate immunity (also called natural or native immunity)
- Provides the early line of defence against microbes.
- It consists of cellular and biochemical defence mechanisms that are in place even before infection and are poised to respond rapidly to infections.
- Fact: Caesarean section may have an impaired immune system in later life due to the lack of exposure to maternal bacteria that would occur during the standard birthing process.
- Adaptive immunity(specific or acquired immunity) system recognizes and reacts to a large number of microbial and non-microbial substances. The defining characteristics of adaptive immunity are:
- Adaptive immunity has two arms: —
- Antibodies: proteins that recognise and bind to antigens. Some of them tend to neutralise it from infecting fresh host cells. Found in serum/Plasma;
- Immuno-globular-M: IgM Antibodies: short-lived – detected 4-7 days after the infection & die after 7 days.
- Immuno-globular-G: IgG Antibodies: formed after 7-14 days and can be detected even weeks/months after the first infection.
- These can be tested by serology test; IgG-specific serology tests work better than IgM.
- T-Cells: Some pathogens adopt other mechanisms to infect host cells, and that is when T-cell immunity may come to the rescue. T-cell immunity is more long-lasting than antibodies. It resides in a subset of white blood cells called T-lymphocytes, or T cells. However, the test for assessing T-cell immunity is complicated and expensive.
- Antibodies: proteins that recognise and bind to antigens. Some of them tend to neutralise it from infecting fresh host cells. Found in serum/Plasma;
- Reinfection: The phenomenon of short-lived antibodies can cause consequent re-infection.
- This is seen in some other respiratory tract viruses.
- The observed protection in the face of non-detectable antibodies highlights the need to study T-cell immunity.
- The Case of COVID-19: In most viral infections, the presence of antibodies in the blood is sufficient to classify individuals as immune. But, antibodies for COVID-19 wane fairly soon. In persons with asymptomatic infections or mild COVID-19, nearly half will have no detectable antibodies after two months.
- Adaptive immunity has two arms: —
- Herd Immunity: It is a form of indirect protection from infectious disease that occurs when a large percentage of a population has become immune to an infection, whether through vaccination or previous infections. This percentage differs for different diseases depending on their degree of infectiousness.
Vaccine:
- Dead/weakened microbes. When they enter the body, it fights & kills them by producing suitable antibodies. Vaccine of Cholera, TB, smallpox, hepatitis; APV (attuned poliovirus)
Solutions to fight communicable diseases
A comprehensive policy must include:
- Vaccination Program: If a vaccine has a proven efficacy in reducing the burden of seasonal influenza, it must be made part of the public health system.
- Universal Healthcare: An umbrella scheme like Ayushman Bharat can easily provide it to everyone using public & private institutions.
- Awareness about Common Etiquettes: Campaigns to educate the public through mass media ahead of the season; especially on respiratory etiquettes and risk reduction.
- Tracking Mutations: For example, There are 41 Virus research Diagnostic Laboratories in India & they can study the nature of infections to provide genetic insights to peer scientists. These findings must be communicated timely.
- Geographical Coverage: India needs a comprehensive programme that covers all states.
- One Health Approach: Assigned coordinated tasks to multiple government agencies involving health, education, environment, and livestock.
- Fighting Vaccine Hesitancy.
| Vaccine Hesitancy |
As per WHO, Vaccine Hesitancy is defined as “reluctance or refusal to vaccinate despite the availability of vaccines” and is influenced by factors such as complacency, convenience and confidence. It’s one of 10 threats to global health.
Factors responsible for Vaccine Hesitancy include:
Popularising scientific thought on the vaccines and debugging the roumers related to vaccine hesitancy are the only ways of tackling it. |